Deep vein thrombosis » DVT
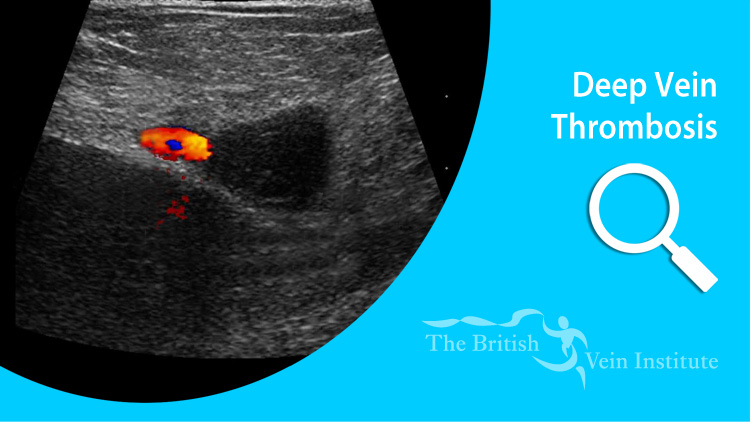
Deep Vein Thrombosis is a condition in which blood clots form in the deep veins of the leg. This may lead to swelling of the leg and is hazardous to life, because bits of clot in the leg may fall off and travel via the main veins to the heart. Here they pass through without a problem, but become stuck in the arteries to the lungs. This is called a 'pulmonary embolism'. This condition causes shortness of breath, collapse and chest pain. Left untreated this may lead to death.
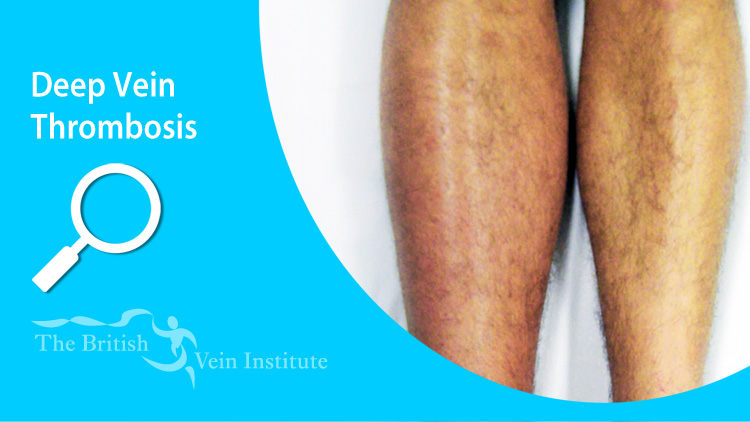
Deep vein thrombosis occurs in about 1 person per thousand per year. It may cause no symptom, but more often leads to pain and swelling in the calf. If the clots spread to the thigh or to the groin both the thigh and calf become very swollen.